What is a cavernoma?
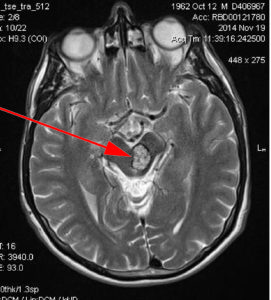
A cavernoma is made up of abnormal blood vessels and can be found in the brain and/or spinal cord and looks like a raspberry.
1 person in 625, in the UK, has a brain cavernoma without symptoms (asymptomatic). This equates to roughly 108,000 people – enough to more than fill Wembley Stadium. A spinal cavernoma is rarer than a brain cavernoma.
A cavernoma is made up of abnormal blood vessels and can be found in the brain and/or spinal cord and looks like a raspberry. Cavernomas are also known as cavernous angioma, cavernous haemangioma or cerebral cavernous malformation (CCM). They can measure from a few millimetres to several centimetres. A cavernoma can get bigger, but this engorgement is not cancerous, and does not spread to other parts of the body. A cavernoma is neither a tumour nor a compression, but a malformation of blood vessels.
Sometimes the cells lining the blood vessels ooze small amounts of blood (inwards) within the cavernoma, or (outwards) into surrounding tissue. The risk of re-bleeding varies widely and is difficult to predict accurately.
Cavernoma also occur in other areas of the body, such as the spine.
Frequency
Figures vary on the frequency of cavernoma.
A commonly cited research study, states that 1 person in 625, in the UK, has a brain cavernoma without symptoms (asymptomatic). This equates to roughly 108,000 people – enough to more than fill Wembley Stadium. A spinal cavernoma is rarer than a brain cavernoma.
Another research study states that asymptomatic cavernoma is more common, giving a prevalence of 1 person in 217. This research also states that 1 person in 2,703 has a symptomatic cavernoma, meaning people who experience symptoms are widely considered to have a rare condition.
With spinal cavernoma, whilst there is no definitive data, there is some research to suggest that approximately 5% of cavernomas are found in the spine, meaning spinal cavernoma is rarer than a brain cavernoma.
A minority of cavernoma, around 20% according to the rare disease resource Orphanet, are thought to be a genetic form and genetic testing can be used to determine whether the cavernoma has a genetic cause or is likely to be random.
Symptoms and diagnosis
Some cavernoma are diagnosed after investigation into other symptoms not definitively linked to cavernoma. These are known as ‘incidental’ cavernoma.
The type, severity, combination and duration of symptoms vary, depending on the location of the cavernoma. Single or multiple cavernomas near the surface of the ‘hemispheres’ or ‘lobes’ in the brain can cause epileptic seizures.
Symptoms may occur after a ‘bleed’ but this is not true in every case. MRI scans are the most reliable diagnostic tool available to determine the presence of cavernoma. It is important, however, that specific scan sequences are used: “T2-weighted” and “gradient echo” (also known as T2-star).
Other diagnostic tools include CT scans and angiography but often these scans cannot be relied upon to show a cavernoma.
Cavernoma are often diagnosed after a person has experienced symptoms which can include
- haemorrhages
- seizures
- headaches
- neurological deficits such as dizziness, slurred speech, double vision and tremors
- weakness, numbness, tiredness, memory and concentration difficulties
Treatment & Management of Cavernoma
Whilst people with cavernoma have things in common, each person remains unique. This should be taken into account for each individual who may require both lifelong support and medical attention. Because cavernoma symptoms can vary widely from person to person, depending on location, number/ size, effective treatment options can vary also. Specific medical advice can only be given by a neurologist, neurosurgeon or other clinical professionals.
Nowadays, diagnosis of cavernoma is invariably made following an MRI scan. What happens next depends on the size and location of the identified cavernoma(s) and the severity of your symptoms. There are currently three main ways of treating cavernoma:
- A ‘wait-and-see’ conservative management approach is often recommended. This will involve treating the symptoms; for example, medication can be prescribed to help control some symptoms such as seizures and pain. You may be advised to have periodic MRI scans to monitor the cavernoma(s). If you have multiple cavernomas, normally associated with the hereditary (familial) form of cavernoma, you will probably be seen by a Clinical Geneticist to determine if there is a genetic cause and then discuss your options.
A major risk with cavernoma is the possibility that it will bleed – what is known as an Intracranial Haemorrhage (ICH). This is a serious bleed that occurs at unpredictable intervals (typically a year or so) which normally results in the cavernoma growing bigger and your symptoms becoming more severe. If your clinician feels that the risk of such a bleed is high, they may recommend that you have one of the two other forms of treatment.
- Surgery to remove the cavernoma. Surgery is a major operation, and more dangerous for cavernoma deep in your brain, especially in your brainstem and spinal cord.
- Radiation treatment, known as Stereotactic Radiosurgery, which zaps the cavernoma with radiation. It is unknown how well cavernomas respond to radiosurgery.
Questions to Ask your Neurologist or Neurosurgeon
If you have an appointment to see a neurologist about your cavernoma it can sometimes be difficult to remember the questions you wanted to ask or know what questions to ask!
Some people find it useful to have a list of questions to take along with them to the appointment. We have prepared some questions, hints and tips at the link below.
